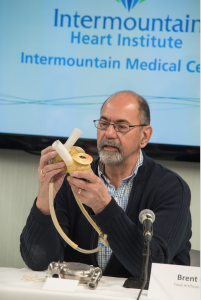
Pioneering Artificial Heart Program at Intermountain Medical Center Celebrates 25 Years of Saving Lives
The most awe-inspiring thing about our program is our patients. It’s incredibly rewarding to see them work so hard to get back to their families and the good lives they had before”
SALT LAKE CITY, UT, USA , May 7, 2018 /EINPresswire.com/ -- Intermountain Medical Center is celebrating a medical milestone: the 25th anniversary of its pioneering Intermountain Artificial Heart Program, which has implanted more than 600 life-saving total artificial hearts and heart-assist devices during the past 25 years.— Bruce Reid, MD, Intermountain Medical Center Artificial Heart Program
The pioneering Intermountain Artificial Heart Program started at LDS Hospital in Salt Lake City in 1993 when James Long, MD, PhD, a young cardiothoracic surgeon, assembled an unusual team of three physicians from different fields to implant the pumps and manage the care for the program’s patients.
The team implanted Utah’s first left ventricular assist device, or LVAD. Since then, the program has implanted 605 devices – life-sustaining heart pumps that help support a failing heart, along with total artificial hearts that replace the native heart – and is now considered one of the premier artificial heart programs in the nation.
Only a few hospitals in the United States implant total artificial hearts.
Among the patients whose live was saved is Richard Morse, one of 50 patients in the world with more than 10 years of LVAD support. Morse was among the first of the trial patients for the HeartMate II LVAD, which was associated with increased survival free from disabling stroke and significantly less major adverse events such as death.
In 1995, the team historically implanted a total artificial heart in Idaho resident Al Marsden, who was the first patient in Utah to receive an artificial heart since Barney Clark, who received the first such implant in the world in 1982. Marsden was supported on the artificial heart for 133 days until a donor heart became available and was successfully transplanted. Today, 23 years later, Marsden is making the most of his gift every day and living in Idaho.
“They tried to explain the artificial heart to me and I didn’t know much about the technology then,” Marsden said. “Because my heart and organs were shutting down, this was my only option. But the doctors told me that no one had survived through the process before long enough to get a heart transplant.”
At that time, pumps were being used for only short periods to support the function of a patient’s heart while they waited for a heart transplant. The Intermountain Healthcare program began pushing the boundaries of how such devices were used — and for how long.
“There were no guidelines back then,” says Brad Rasmusson, MD, a critical care specialist and Thoracic ICU Medical Director for the Intermountain Medical Center Artificial Heart Program who was an original member of the team, along with Dr. Long and Cris Cowley, MD, an anesthesiologist. “We didn’t know how patients would respond.”
Very well, it turned out.
In the past 25 years, the Intermountain Artificial Heart Program at the Intermountain Medical Center Heart Institute has been one of the most active centers in the country and is a national leader in extending lives, conducting critically important research, and testing experimental devices that are now being used around the world. It’s one of only a few elite programs across the country that implants total artificial hearts, mechanical devices that replace the native heart entirely rather than just assist it, while the patient awaits a transplant.
Other milestones realized by the Artificial Heart Program at the Intermountain Medical Center Heart Institute include:
The program’s team has implanted 605 total devices (398 long-term and 207 temporary)
Its patients consistently meet or exceed national averages for survival.
The program has implanted 232 devices that bridge patients to a heart transplant and 110 devices that serve as destination (permanent) therapy
It was the first program in the nation to implant the HeartMate II as a permanent therapy in 2004.
It was the first program in Utah to implant the HeartWare HVAD device, the smallest LVAD pump on the market today.
It became the largest participant in a ground-breaking national study on using LVAD therapy as a permanent treatment for patients who were fatally ill but ineligible for a transplant.
Today, the team has grown from three doctors to more than 40 caregivers, each with a direct role in the care of nearly every patient who enters the program. Patients who are cared for by the team suffer from advanced heart failure, which occurs when the heart can’t properly move blood throughout the body. The most common causes of heart failure are coronary artery disease, high blood pressure, and diabetes. Doctors manage heart failure with medication and dietary changes, but there’s no cure.
“We use cutting-edge technology and equipment to save lives, but the program is very much about dedicated people caring for patients who are very sick and in great need of support. It’s incredibly satisfying to help these patients regain the lives they once enjoyed,” says Bruce Reid, MD, Mechanical Circulatory Support Surgical Director of the Intermountain Medical Center Artificial Heart Program.
Mechanical pumps relieve strain on a damaged heart by doing most, or all, of its work. They’ve become smaller and more durable over the years, and some can even be inserted via a catheter, without the need for a large incision in a patient’s chest.
An LVAD doesn’t replace the heart. Instead, it’s a mechanical heart pump that assists the left side of the heart in pumping blood, nutrients, and oxygen to the rest of the body. LVADs have both internal and external parts. Patients must be connected to battery or AC power at all times.
“This is the most complicated therapy in medicine today — but the most awe-inspiring thing about our program is our patients,” says Dr. Rasmusson. “People can come back from heart failure, and the result is life-changing for them and their family. It’s incredibly rewarding to see them work so hard to get back to their families and the good lives they had before.”
Jess Gomez
Intermountain Medical Center
801-507-7455
email us here
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.